US Debt Limit Suspended into 2025; Neither Side Gets Everything It Wanted
President Joe Biden and House Speaker Kevin McCarthy (R-CA) both claimed victory last week after Congress approved a 99-page bill that suspends the nation’s debt limit into 2025. The legislation passed the US House overwhelmingly, 313-117, with 71 Republicans voting “no”, while 46 Democrats also opposed the bill. Subsequently, the Senate passed the legislation 63-36, sending the bill to the President for his signature. While the political maneuvering gained headlines, some substantive policy issues were at play. Here’s a quick look at some key provisions:
1) Veterans Health Care Funding – Democrats attempted to portray the GOP as targeting military veterans by supporting some cuts in Biden’s veterans’ health care funding. There were no cuts in the final package.
2) Unspent COVID Funds – The bill rescinds about $30 billion in unspent coronavirus relief money that Congress approved through previous bills. It claws back unobligated money from dozens of federal programs that received aid during the pandemic, including rental assistance, small business loans and broadband for rural areas. The legislation protects pandemic funding for veterans’ medical care, housing assistance, the Indian Health Service, and some $5 billion for a program focused on rapidly developing the next generation of COVID-19 vaccines and treatments.
3) Public Assistance Work Requirements – While the GOP House leadership wanted to go further to require broader work requirements, the final agreement included modest changes, requiring more able-bodied Temporary Assistance to Needy Families (TANF) and Supplemental Nutrition Assistance Program (SNAP) recipients to actively seek employment. Biden succeeded in getting expansion in other programs included in the final deal. Passage of the so-called “Fiscal Responsibility Bill” means the US will not default on its loans this week, but as many observers note, it delays a more comprehensive federal budget reckoning.
Nevada Lawmakers Pass First State Bill to Cap Drug Prices at HHS-Negotiated Rate; Governor Vetoes Measure
Nevada legislators, on an almost party-line vote, passed first-of-its-kind legislation in late May to link what state payers will pay for prescription drugs to that which is negotiated by the federal government. However, on June 5, Governor Joe Lombardo (R) vetoed the measure. The Inflation Reduction Act (IRA), signed in last August, gave the US Secretary of Health and Human Services the power to negotiate drug prices with manufacturers to establish the maximum price of drugs sold to Medicare recipients. The Nevada legislation proposed to use that price for all state-regulated health plans. Federal negotiations will set prices for 10 drugs in 2026, another 15 in 2027, another 15 in 2028 and another 20 in 2029. Health and Human Services officials will select the drugs to negotiate from about 50 drugs with the highest Medicare spending and consider production cost and distribution, time on the market (at least seven years) and data on pending and approved patent applications. The initial list of 10 drugs will be released in September, which will then mark the beginning of negotiations. The legislation also stipulated that any company or individual found to be selling prescriptions at a price higher than the maximum fair price would be in violation of deceptive trade practice laws and face civil actions. While the Nevada legislation passed with comfortable margins, Governor Lombardo vetoed the bill. In his veto message, the governor said the state shouldn’t rely on a federal process (with no state input) to determine drug prices and argued that government price controls on prescription drugs would negatively impact medical innovation, leading to fewer new therapies for patients. Democrats did not have enough votes to attempt to override the veto. Governor Lombardo’s relatively lengthy veto message of the “Affordable Medicine Act” can be found here. Legislators in Connecticut and Maine considered similar legislation in 2023, but it did not advance.
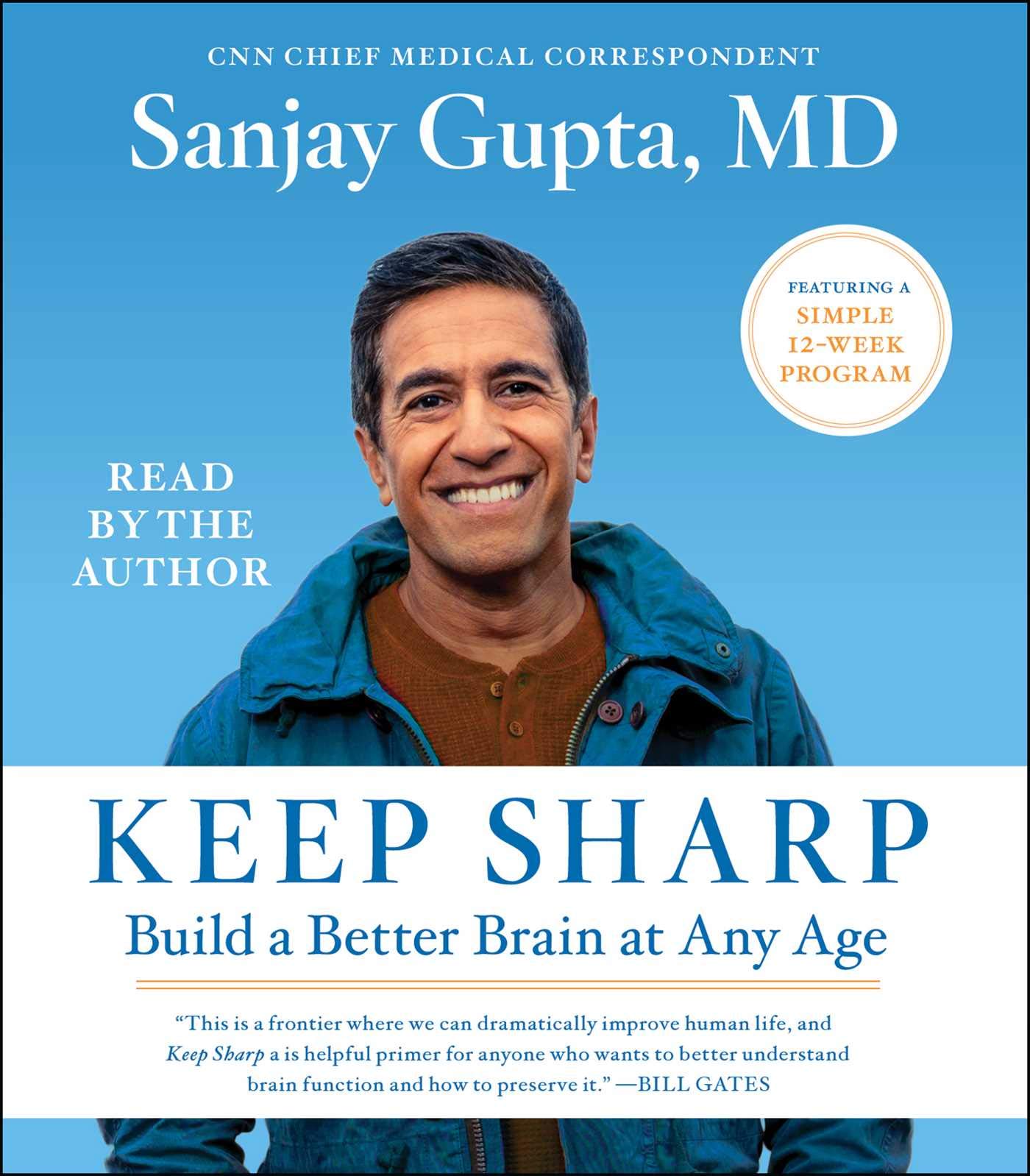
Minnesota Becomes Latest State to Pass “Prescription Drug Affordability Board” Legislation: Potentially Nation’s Most Powerful PDAB
Minnesota drug pricing reform advocates are celebrating a long-awaited victory, as Governor Tim Walz (D) signed legislation creating the state’s first PDAB. The Board will have seven voting members appointed by the Governor and two non-voting members appointed by legislative leaders. It will hire an executive director and other staff and hold public meetings every three months. An 18-member advisory council will also be appointed by the Governor. Pharmaceutical manufacturers receive one seat on the advisory council, as will health plans, pharmacy benefit managers, employers, researchers, rare disease advocates, pharmaceutical distributors and wholesalers. Patients and consumers receive two seats and health care providers receive three. The council has the authority to review any brand name drugs or biologics with a WAC increase of more than 15% or more than $3,000 during any 12-month period or any product with a WAC of $60,000 or more per calendar year or course of treatment. This broad language opens up hundreds of medications and therapies for potential review. If the PDAB finds that the drug creates affordability challenges, it has the authority to set an upper payment limit (UPL) for the medication. Many argue that the law creates one of the most powerful state drug affordability boards in the nation. Previous efforts to pass PDABs in the state have fallen short, but newly established Democratic majorities in both houses changed the fate of the legislation.
Value-Based Pricing Agreements: Bipartisan (sort of) Support Moves House Bill Forward
Republican members on the House Energy & Commerce Committee unanimously supported H.R. 2666, the Medicaid VBPs for Patients (MVP) Act, during markup on May 24. However, Democrats were divided, with the vast majority voting no on final passage. The MVP Act codifies existing protections for companies to enter into value-based purchasing agreements under the Medicaid program. The bill was led by Rep. Brett Guthrie (R-KY) and Anna Eshoo (D-CA). Only two other Democrats stood with Eshoo and the Republicans in advancing the measure 31-19. Other Democratic supporters were Reps. Tony Cárdenas and Scott Peters also of California. The bill would codify the current Centers for Medicare and Medicaid Services rule that was designed to remove regulatory obstacles to value-based contracting in commercial health plans by allowing more flexibility in Medicaid rules around reporting “best price.” Some Democrats believe that any increased flexibility for manufacturers would negatively impact state Medicaid programs and potentially increase costs. Republicans argued that the focus is on ensuring access to transformative therapies. “I feel this bill will not lower the cost of prescription drugs and could in fact increase drug costs to state Medicaid programs and the federal government and for these reasons I can’t support the bill,” said Rep. Frank Pallone, the ranking Democrat on the Energy and Commerce Committee. Supporters of the bill argued it will help Medicaid programs afford very high-cost treatments like cell and gene-based therapies. “This bill is about access. And it would ensure that Medicaid patients have the same access to game-changing novel gene therapies and the long-term benefits and improved quality of life that they provide as those patients with private insurance,” said Rep. John Joyce (R-PA). The bill now moves to consideration by the full House.
Gridiron Public Affairs on Spotify
Learn more about Gridiron Public Affairs by listening to the “House Call” podcast sponsored by Affinity Strategies. Greg Chesmore, Gridiron’s CEO, discussed strategies for shaping health care policy with host Claire Vincent.